Colorectal / Proctology
What is GI surgery?
GI surgery, otherwise called Surgical Gastroenterology is a superspeciality dealing with diseases of the abdominal organs, mainly involved in nutrition and digestion of food which may require surgical management most of the times. M.Ch /DNB (Surgical gastroenterology) are the courses recognized by Medical Council of India for this superspeciality and can be registered with them. As eating a normal diet with a good digestion is essential for everyone, even non critical diseases require a proper diagnosis and treatment.
Why to consult GI surgeon / Surgical Gastroenterlogist?
The 3 year rigorous training involved in the course focuses only on the disorders of the digestive (Gastrointestinal) system. Hence they are very experienced in dealing with them as they are well-versed in their presentation, diagnosis and treatment. They are actively involved in the surgical procedures in large numbers pertaining only to the abdomen and manage them postoperatively. They recognize and manage complications early, if arise, as they have the immaculate capacity to identify and treat them.
When to consult a GI specialist?
The common symptoms which may require a consultation of GI surgeon are
- Abdominal pain
- Indigestion / Reflux of food
- Recurrent Vomiting / blood vomiting
- Abdominal bloating or distension
- Any swelling in the abdomen / groin
- Jaundice
- Blood / mucus in motion
- Altered bowel habits (Constipation / Diarrhoea)
Content will be available soon...
Content will be available soon...
Content will be available soon...
An anal fissure (fissure-in-ano) is a small, oval shaped tear in skin that lines the opening of the anus. Fissures typically cause severe pain and bleeding with bowel movements. Fissures are quite common in the general population, but are often confused with other causes of pain and bleeding, such as hemorrhoids
Anal fissures can occur at any age and occur equally in males and females. Most (85-90%) fissures occur in the posterior (back) midline of the anus with about 10-15% occurring in the anterior (front) midline.
WHAT ARE THE SYMPTOMS OF AN ANAL FISSURE?
The typical symptoms of an anal fissure include pain and bleeding with bowel movements. Patients note severe pain during, and especially after a bowel movement, lasting from several minutes to a few hours. Patients often notice bright red blood from the anus dripping into the pan. Between bowel movements, patients with anal fissures are often relatively symptom-free. Many patients are fearful of having a bowel movement and may try to avoid defecation secondary to the pain.
WHAT CAUSES AN ANAL FISSURE?
Fissures are usually caused by trauma to the inner lining of the anus. A hard, dry bowel movement is typically responsible, but loose stools and diarrhea can also be the cause. The inciting trauma to the anus produces severe anal pain, resulting in anal sphincter spasm and a subsequent increase in anal sphincter muscle pressure. The increase in anal sphincter muscle pressure results in a decrease in blood flow to the site of the injury, thus impairing healing of the wound. Ensuing bowel movements result in more pain, more anal spasm, diminished blood flow to the area, and the cycle is propagated. Treatment strategies are aimed at interrupting this cycle to promote healing of the fissure.
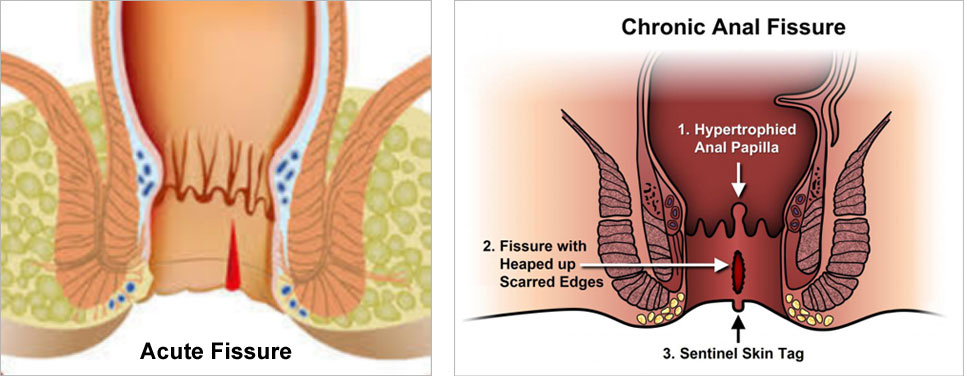
Anal fissures may be acute (recent onset) or chronic (typically lasting more than 8-12 weeks). Acute fissures may have the appearance of a simple tear in the anus, whereas chronic fissures may have swelling and scar tissue present. Chronic fissures may be more difficult to treat and may also have an external lump associated with the tear, called a sentinel pile or skin tag, as well as extra tissue just inside the anal canal, referred to as a hypertrophied papilla.
Quite commonly, anal fissures are misdiagnosed as hemorrhoids by the patient or the primary care physician due to some similar symptoms between the two. This delay in diagnosis may lead to an acute fissure becoming a chronic one and, thus, more difficult to treat. Misdiagnosis of an anal fissure may also allow other conditions to go undetected and untreated, such as serious infections or even cancer.
WHAT IS THE TREATMENT OF ANAL FISSURES?
The majority of anal fissures do not require surgery. The most common treatment for an acute anal fissure consists of making one's stool more loose and bulky with a diet high in fiber .Stool softeners and increasing water intake may be necessary to promote soft bowel movements and aid in the healing process. Topical anesthetics, such as lidocaine, can be used for anal pain and warm tub baths (sitz baths) for 10-20 minutes several times a day (especially after bowel movements) are soothing and promote relaxation of the anal muscles, helping the healing process. These non-operative measures will help achieve resolution of pain and bleeding and, potentially, heal greater than half of acute fissures with virtually no side effects.
Other medications may be prescribed that promote relaxation of the anal sphincter muscles. Acute fissures with severe sphincter spasm may require surgical procedure under anaesthesia to loosen the sphincter muscle to aid in easing the pain and accelerate healing . Chronic fissures are generally more difficult to treat, and your surgeon may advise surgical treatment either as an initial treatment or following attempts at medical management.
Content will be available soon...
Content will be available soon...
Content will be available soon...
